Depression in Developing Countries
BY SREEJA KODALI for YALE GLOBAL HEALTH REVIEW
In his book The Noonday Demon: An Atlas of Depression, Andrew Solomon, describes the “worst case of depression” he had ever seen. Maggie Robbins, charming and “always so lustrous with energy,” in her deepest depression, was “curled up on the couch in a tight ball, wincing as though someone were putting slivers of bamboo under her fingernails.” She could barely speak; yet despite her lowest lows, Maggie was successfully treated for her depression with therapeutic medications like Depakote, lithium, and Wellbutrin. Maggie now writes poetry, makes art, and works a day job as a copy editor.1
The National Institute of Mental Health defines depression as a serious but common illness characterized by prolonged periods of sadness that interfere with, or at worst, wreck daily life.2 According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, a diagnosis for major depressive disorder requires either symptoms of a depressed mood or loss of interest and pleasure, along with four other symptoms such as changes in weight, sleeping patterns, fatigue, feelings of worthlessness, or suicidal thoughts.3 Although not fully curative, the treatment of depression has greatly progressed.4 As Solomon describes it, “Depression these days is treatable; you take antidepressants like you take radiation for cancer.”1 Maggie – who had once been so affected that she would “lay in a corner, not stirring for days at a time” – is a dynamic testament to the improvement of depression treatment.
Today, many therapies for depression are highly effective. Psychotherapies such as Cognitive Behavioral Therapy and interpersonal therapy teach patients positive thinking strategies and coping mechanisms. In mild to moderate depression, these therapies alone can suffice as treatment.6 For more severe cases, therapy can be supplemented by a variety of medications – selective serotonin reuptake inhibitors (SSRI), serotonin and norepinephrine reuptake inhibitors (SNRI), monoamine oxidase inhibitors (MAO), and tricyclics.2 Depending on the patient’s needs, physicians may prescribe antidepressant medications. Aside from therapy and antidepressants, brain stimulation therapies can be used. During electroconvulsive therapy – the oldest and most well documented procedure – patients have an electric current passed through their heads.5 Although how this treatment works to combat depression is not well understood, research shows that it can be effective.7,8,9
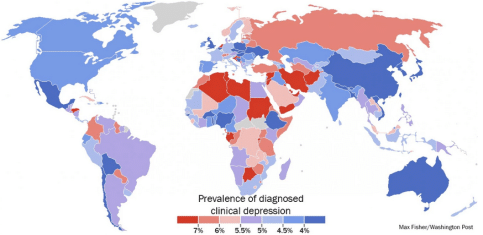
But what about in situations where there is limited access to doctors, specialists, and treatment options? Maggie was fortunate: as she became more depressed, a friend was able to get her back on medications from a psychiatrist. What if there was one psychiatrist per one million people, three million people, or ten million people, as is the case in Uganda, Zambia, and Indonesia respectively?10 This is a reality in multiple developing nations, where less than ten percent of afflicted people receive treatment for depression.11 The need for therapeutic treatment is overwhelming: worldwide, over 350 million people are estimated to suffer from depression.11 In a study conducted in rural India, 430 people out of every thousand at-risk individuals were depressed – almost half.4 In another study in rural regions of India, 39.6 percent of the entire population suffered from mild to moderate depression.12 Untreated depression is indeed a global crisis.
We can better understand the global impact of depression by measuring it in terms of disability. When analyzed by the disruption and dysfunction it causes in peoples’ lives, depression is the leading cause of disability worldwide.11 A collaborative report between the World Health Organization, World Bank, and Harvard School of Public Health measured the global burden of disease using DALYs (disability adjusted life years). This study revealed that while not typically fatal, depression is the current—and rising—leader in silently stealing years of productivity, health, and life from the world’s population.13
One of the many individuals suffering from mental illness in developing nations is a young man in Aceh, Indonesia. In his early thirties, the young man “has been [mentally] sick for as long as anyone could remember,” according to Mahdi Abdullah, a village leader.14 But the young man’s condition worsened when armed conflict arrived in the area, as Aceh province attempted to achieve independence from Indonesia.15 He was beaten twice by the Indonesian soldiers. He “stopped working, which worsened the already tenuous economic situation for his mother and grandmother, with whom he lives.”14
This young man’s story reflects the role of conflict as a unique trigger of depression in developing nations. In a literature review published in the Journal of the American Medical Association of 161 articles reporting surveys from over 80,000 refugees, researchers found that exposure to torture and other potentially traumatic events accounted for higher reported rates of depression.16 Specifically, several conflict-related factors – potentially traumatic events, reported torture, and residency status –were correlated with higher rates of depression. In the most recent conflicts in Syria, the international NGO Doctors Without Borders reported that Syrian refugees resettled in Lebanon have been left feeling fearful, insecure, uncertain, and economically unstable.17,20 In adults, depression and anxiety were the most common diagnoses.17
Aside from conflict, other triggers of depression in developing nations are disease, poverty, and the struggle of difficult daily lives. In a study conducted in rural Uganda, areas significantly affected by HIV and AIDS saw a 21% rate of depression.18 But even developing areas not devastated by disease had similar rates of depression. A combination of difficulty of daily tasks, financial instability, shelter and food insecurity, and loss of children can lead to depression. In a study conducted in rural Pakistan, half the women tested suffered from depression and anxiety.19 Researchers discussed social climate as an explanation for this high rate, pointing to early marriage, early motherhood, multiple pregnancies, and adjusting to life with in-laws as possible factors.
Just as depression is a significant issue in developing nations, so too is the lack of resources and treatment opportunities. In 2001, the World Health Organization published a report documenting the available mental health resources by country in all its member states, covering 98 percent of the world population.10 Their report, the Mental Health Atlas, revealed the disparity in facilities, resource accessibility, human resources, access to medication, and documented records for mental health across the globe. The report also showed severe mental health resource scarcity in developing nations compared to the rest of the world. In the United States, for instance, mental health policy exists and is mentioned particularly in the general health plan. Though the complicated American healthcare system has made it difficult for some patients to cover the costs of mental healthcare, the expansion of insurance-based financing through the Affordable Care Act is improving access to care. People in the United States also have access to thousands of well-equipped mental health facilities. There is a psychiatrist for every 12,000 Americans, a specialized nurse for approximately every 32,000 people, a psychologist for every 3,400 people, and a social worker for roughly every 5,500 people.10 Similarly, the United Kingdom has mental health plans and policies, with mental health featuring prominently in their general health policy. More than ten percent of their total health budget, financed by the government, is dedicated towards mental health. As for human resources, the country is well-staffed: a psychiatrist for every 5,652 people, specialized nurse for every 1200 patients, psychologist for every 7,800 people, occupational mental health therapist for every 3,500 people, and many more mental health workers.
In developing nations, numbers are relatively grim. In Uganda, for example, specific mental health policy does not exist and mental health is not mentioned in the general health policy. Government funding for mental health does not exist. There are a grand total of 28 mental health outpatient facilities in the entire nation. Ugandans face an alarming dearth of mental health professionals and workers: one psychiatrist for more than a million people, one mental health care nurse for every 130,000 people, one psychologist for every five million people. In Indonesia, although mental health policy exists and is mentioned in the general plan, no funding is available through the government. The country lacks human resources as well. The only available mental health worker statistic was for psychiatrists: one for every ten million people, or just 23 in the entire nation.10 As frightening as these numbers seem, other nations are even worse off. Sierra Leone and Liberia, both classified as a least developed nation according to the United Nations21 and reeling from a traumatic Ebola epidemic, each only have one psychiatrist in the entire country.10 Sierra Leone has no mental health facilities; Liberia has one.
Limited resources for mental health, especially human resources, pose great challenges to treating depression in developing nations. Conventional treatment options like medications prescribed by psychiatrists and sessions with therapists – therapies that helped Maggie – are simply not possible without mental health professionals. So what can be done in countries lacking these resources? Just like in other global health treatment deliveries, depression treatment must be modified for large-scale delivery to areas with limited resources. Depression treatment in developing countries should be “available, accessible, cheap, culturally appropriate, convenient, and non-stigmatizing.”22 Large advances have made depression treatable for Maggie. And further progress is underway to make similar success stories for those in underdeveloped nations.
One treatment option is talk therapy facilitated by laypersons instead of experts. Talk therapy, also known as psychotherapy, is a common treatment for depression that teaches patients how to deal with negative thoughts and manage stress. The two most common types are cognitive-behavioral therapy, involving healthy changes in one’s thoughts and actions, and interpersonal therapy, which target a person’s communication and interactions with people.6 Conventionally, a professional psychologist, psychiatrist, social worker, counselor, or therapist would administer talk therapy. Where such professionals are few, studies have shown that cognitive behavioral strategies facilitated by non-professionals were highly effective. For instance, in the rural outskirts of Rawalpindi, Pakistan, local health education workers, called Lady Health Workers, were trained to teach the Thinking Healthy Program. This program used principles of cognitive-behavioral therapy and active listening. The Lady Health Workers visited and taught the program to expecting mothers in addition to the maternal and childcare educational lessons they normally gave. A survey of depressed mothers showed that the program significantly reduced depression and disability rates. And the health workers, the facilitators of the mental health techniques, were not professionals; they had only completed secondary school.23 In Goa, a part of western India, a similar intervention program for treating depression – the largest intervention in a middle- or low-income country – was tested in primary care facilities. A layperson counselor underwent two months of training before administering the intervention treatment, which consisted of psychoeducation, “strategies for symptom alleviation,” and information for other resources. The intervention was extremely impactful: there was a 30% reduction in depression and anxiety disorders.24
The shift from professionals to laypersons in treating in underdeveloped, human-resource-challenged places is not novel. It is called task shifting. Task shifting, according to the World Health Organization, is the “process of delegation whereby tasks are moved, where appropriate, to less specialized health workers.”25 And the strategy has proven itself effective in combatting HIV and AIDs where health workers are short but the disease is widespread.25 In these areas, treatment administered by less qualified workers is better than no treatment at all.
Global health experts are successfully applying task shifting to the treatment of depression. One specific, task-shifted form of talk therapy that has been developed is Group Interpersonal Therapy, or GIPT. True to its task-shifting roots, this modified form of talk therapy is facilitated by non-professionals. Unlike the aforementioned studies, GIPT was inspired by the second branch of talk therapy, interpersonal therapy. While interpersonal therapy is normally conducted one-on-one, GIPT operates in a group but focuses on improving human interaction to treat depression. In Uganda, GIPT sessions were led by locals who had undergone two weeks of training. The patients receiving GIPT drastically improved in comparison to the control group. Where the control group saw around a 40 percent reduction in depressive symptoms, the intervention group saw almost an 80 percent reduction.26 A New Jersey-based organization called Strong Minds implemented the GIPT intervention model from this study in other regions of Uganda. After sixteen weeks of group interpersonal therapy, Strong Minds saw incredible results: 94 to 97 percent of patients were found to be depression-free.27 Their mental health facilitators had been trained for just ten days in GIPT.
Depression is global, medical issue – not just for citizens of the developed world, but also for millions of people in developing nations. Although depression may be misperceived as a “first-world problem,”22 it is an international problem and the world’s greatest burden of disease. For many residents of developing nations, life presents a host of unique triggers such as conflict and disease epidemics, in addition to more conventional and day-to-day challenges. As a result, depression in developing nations is equally prevalent as—and often more prevalent than—depression in wealthier nations. Developing nations also struggle with a great dearth in resources for mental healthcare, particularly trained and empathetic human resources. In order to combat depression in developing nations, task-shifting of cognitive behavioral and group interpersonal therapy to health workers is being tested and has proven highly effective in reducing depression and disability. Hopefully, as more treatment plans and ideas are implemented, depression can be tackled at a global scale so that mentally unwell people like Maggie and Aceh can receive the care they need, regardless of where they live.
Read more online at the Yale Global Health Review.